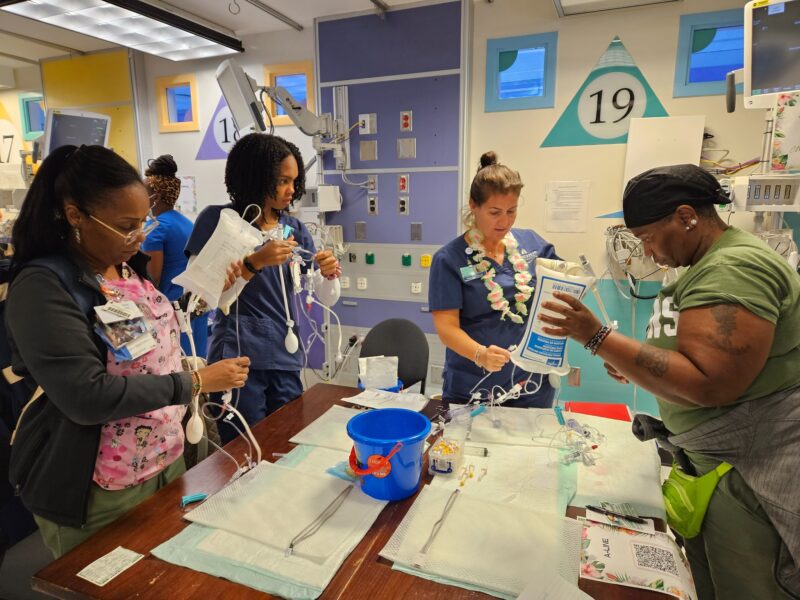
Biocontainment Unit’s coordination and preparedness drills help spread leadership across the hospital.
It’s 6 a.m. on a random Saturday morning when the phone rings. Are you ready? Is your dog?
Of course. You’re part of the nursing response team for the Biocontainment Unit, or BCU, at the Johns Hopkins Hospital. “All hospital disaster plans are built on nurses responding,” insists Neysa Ernst, MSN, RN, nurse manager of the BCU on Osler 8. Adds Jade Flinn, MSN, RN, nurse educator for the BCU, the next big outbreak “is not going to happen on Monday at 10 a.m.” Hence the timing of the no-notice drills and training completed at least quarterly.
Flinn explains that her job boils down to three S’s: The space; the stuff; the staff.
The space is the 7,900-square foot BCU, with three patient rooms, a lab, showers and “don and doff” areas for putting on and removing personal protective equipment. Waste is sterilized and kept out of the main hospital disposal stream, and the ventilation system is separate as well.
The stuff is any supply the team could possibly need, when stepping out for more isn’t an option.
The staff is 30 nurses—led by Ernst—recruited from units across the hospital, who collaborate with critical care physicians, infectious disease specialists, and infection control epidemiologists to best care for patients on the BCU.
[Read a profile of Neysa Ernst, DNP student.]
Flinn’s role in the room? “I was also trained as a neuro ICU nurse, so I’m used to making sure the patient is calm, cool, and collected so that we can deliver the most efficient and safe care.” All while she’s churning inside: “I’m an adrenaline junkie. … The ultimate reward is obviously to go through one of these things [successfully isolating and treating patients with highly contagious illnesses].” But knowing she’s got all three S’s handled—and the team does too—is nearly as big a thrill as saving a life.
(At the publication deadline for this magazine, COVID-19 was continuing its spread across the globe but had not brought its first patient to the BCU. “Our hospital and BCU are in full swing continuing to prepare for an influx of patients as the number of confirmed COVID-19 patients rises in Maryland and our surrounding states,” Flinn reported.)
Not everyone is cut from the same cloth as Ernst and Flinn, and they understand that. They don’t want to judge. They want to be able to depend on you, period. “We ask them, ‘Who’s going to take care of your dog?’ Get all those things worked out,” Ernst says.
Team members self-select, with Ernst asking for a two-year commitment at minimum for the sake of continuity. Word of mouth from those who’ve been on the team is invaluable. But Flinn also isn’t above a little recruiting via swag. “We have this really cool gear with our logo on it. People are, like, ‘Hey, that’s a really cool T-shirt.’ ” The team member then gets to rave about the experience.
Not all organizations work this way. Ernst points out a hospital whose ICU nurses are simply expected to be on call for biocontainment duty. That’s far easier, of course. “We are so lucky to have an institution that understands the model.”
BCU nurses continue working in their regular positions throughout the hospital, which Flinn says makes all the drills and training in the BCU even more valuable to the overall institution. “We give back to Johns Hopkins by preparing 30 nurses with disaster planning experience who grow as leaders in their own departments all a cross the hospital.”
The BCU serves the U.S. Department of Health and Human Services Region 3, which includes Delaware, Maryland, Pennsylvania, Virginia, West Virginia, and Washington, DC. It’s a lot of space to cover, which brings in Johns Hopkins Lifeline to transport patients to East Baltimore and through the bowels of the hospital to Osler 8. Yes, it’s intense. It’s where all the training and coordination pay off. Space, stuff, and staff, with nothing taken for granted. “We even have special containment devices for [transporting] patients so that if one of them were to vomit, for instance, it would not get into the environment,” explains Flinn.